1000/1000
Hot
Most Recent

Cardiac rehabilitation is a multidisciplinary program that includes psychoeducational support in addition to physical exercise. Psychoeducational intervention is a component that has had accelerated interest and development in recent decades. The aim was to analyze the current evidence on the effectiveness of psychoeducational interventions for patients with acute coronary syndrome (ACS).
Acute coronary syndrome (ACS) is the most common disease that requires acute cardiac care, being associated with a high risk of morbidity and mortality and a severe impact on patients and healthcare systems [1]. ACS refers to a spectrum of clinical presentations that include both myocardial infarction (MI) with ST-segment elevation (STEMI) and without ST-segment elevation (NSTEMI) and unstable angina (UA) [2]. The most common pathophysiological mechanism involved is coronary atherosclerotic plaque disruption complicated with thrombosis [3]. Modifiable risk factors for coronary thrombosis are usually hypertension, smoking, diabetes, hyperlipidemia, and obesity, while age, male sex, family history, and ethnicity are the unmodifiable ones [4]. From a morphopathological point of view, the underlying element is cardiomyocyte necrosis for MI, or myocardial ischemia without cell destruction in UA [5]. Cardiac rehabilitation (CR) is a multidisciplinary program whose core components must include psychosocial support and patient education in addition to physical exercise, modification of the cardiovascular risk factors, and dietary counseling [6]. The customization of the program for specific cardiac manifestation started in 2010 when the key steps to deliver CR were established [7]. The latest guidelines of the European Society of Cardiology (ESC) highly recommend that patients with ACS to follow a rehabilitation program [8]. In the modern era, the most notable proven benefits are a 26% reduction in cardiac mortality and an 18% reduction in recurrent hospitalization [9].
Depression and anxiety after an MI develop in 30–40% of patients [10], with both being associated with substantial increases in the risk of adverse cardiovascular outcomes [11][12]. Psychological interventions can reduce the prevalence of emotional disorders, with relaxation training [13], stress management [14], and low-level cognitive behavioral therapy (CBT) techniques [15] being recommended in the CR program. In addition, metacognitive therapy for distressed CR patients might be suitable [16], and problem-solving therapy for depressed patients can also bring additional benefits [17]. Another psychological approach with success in eliciting behavioral change (initiating an exercise regimen and changing dietary habits) [18] and increasing physical activity [19] is motivational interviewing. Associated with psychotherapy, patient education should be integrated into the CR program for it to be complete [20]. Although current data indicate that education-based interventions have no effect on total mortality, total revascularizations, and hospitalizations, the main benefit obtained is the reduction in fatal MI and/or non-fatal cardiovascular events [21].
We consider this systematic review of valuable importance due to its extensive research and, as far as we know, it is the first to evaluate the benefits of psychoeducational rehabilitation focused on acute coronary syndrome. In addition, our paper presents the role of an intervention to prevent emotional disorders such as depression, anxiety, and post-traumatic stress syndrome.
Other systematic reviews in the field provide substantial data on the positive effects of psychological and educational interventions in patients with cardiovascular disease, the most narrow group investigated being one that included patients with coronary artery disease (CAD) [10][21][22][23][24][25][26]. Starting from the fact that the negative psychological effect of acute myocardial infarction is more important compared to that in stable ischemic heart disease [27], we considered it necessary to analyze studies that included only patients with acute coronary syndrome.
The aim was to analyze the current evidence on the effectiveness of psychological and educational interventions (as an isolated measure or in a cardiac recovery program) compared to the usual care exclusively for patients with acute coronary syndromes. We aimed to summarize the dose and types of interventions currently administered and their benefits for rehospitalization and quality of life, but also the control of the cardiovascular risk factors, exercise capacity, and adherence to cardiac rehabilitation. We also considered it important to include the understanding and attitude towards the disease, as well as the effects on psychological and medical symptoms.
To our knowledge, this systematic review is the first that aimed to summarize the evidence regarding the impact of psychoeducational rehabilitation in patients with ACS. More specifically, the provided data are clearly promising in terms of the utility of these interventions to improve hard endpoints as well as the quality of life, including alleviation of symptoms of depression and anxiety. Taking into account the heterogeneity issue of the included studies, we emphasize the need for large RCTs with structured integrated multi-modality psychological interventions with a detailed methodology of implementation. By presenting in detail the interventions used in the included randomized controlled trials (type of psychotherapy, number of sessions, and total dose performed) and thus by exposing their heterogeneity, we propose a personalized medicine approach in the psychoeducational rehabilitation of ACS. The benefits of psychoeducational interventions on different aspects of cardiac rehabilitation programs are illustrated in Figure 1.
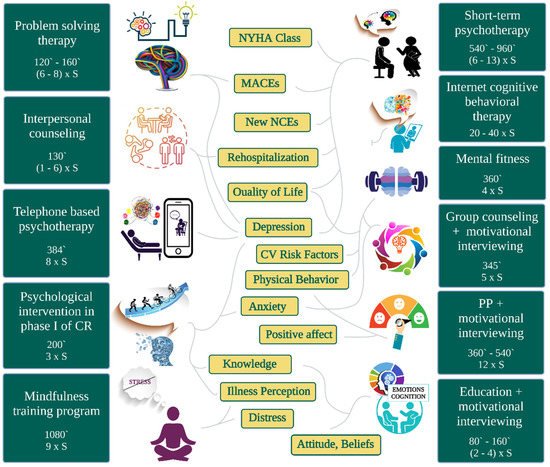
Figure 1. The benefits of psychoeducational interventions specific to the type of cardiac rehabilitation programs and their total dose expressed in number of sessions (S) and minutes (`). CR = cardiac rehabilitation, PP = positive psychology, NCEs = non-cardiovascular events.
Most studies in the field enrolled patients without a determination of various mental health comorbidities with ACS before the intervention. The literature presents a minority of trials that divided the intervention group into two subgroups: with and without comorbidity. We did not find any RCT that studied the benefits of a psychoeducational intervention applied only to patients without a mental disorder diagnosed with ACS. This is an important area for future research, taking into account a substantial increase in the prevalence of mental health disorders among patients with acute MI, according to Sreenivasan et al. [28]. Particularly for depression, a multifaceted and bidirectional relationship with cardiovascular disease is described, especially with ACS [29]. Thus, depression by itself may be the cause of MI, but it is not known whether psychoeducation in this category of patients has similar benefits to the same intervention in patients without depressive symptoms. Meta-analyses in this field have demonstrated the benefit of psychological intervention on mortality and morbidity in CAD [11][23][24][25][26][27]. The latest update of the most rigorous reviews (by Cochrane Collaboration) [25] showed the benefit in the current era of optimal psychoeducational intervention. Regarding prognostic outcomes, the positive clinical outcome that resulted from the analysis was for cardiac mortality (RR 0.79, 95% CI 0.63 to 0.98). In contrast, no obvious effect was demonstrated in terms of risk reduction for total mortality (RR 0.90, 95% CI 0.77 to 1.05), rates of revascularization (RR 0.94, 95% CI 0.81 to 1.11), and rates of non-fatal MI (RR 0.82, 95% CI 0.64 to 1.05). The meta-analysis has revealed a reduction in depressive symptoms (SMD −0.27, 95% CI −0.39 to −0.15), anxiety (SMD −0.24, 95% CI −0.38 to −0.09), and stress (SMD −0.56, 95% CI −0.88 to −0.24) in the intervention group compared to the comparator group. In addition, by direct comparison of the studies, the authors demonstrated positive effects on health-related quality of life, type A behavior, and vital exhaustion. Moreover, the systematic review of Reid et al. [11] completes the data from the literature and shows the benefits of psychological intervention on blood pressure for patients. Furthermore, the authors describe a positive effect on knowledge and satisfaction for both patients and their partners. As demonstrated in the Cochrane review [22], education-based intervention in CAD reduced fatal and/or non-fatal cardiovascular events (other than MI) compared to control groups receiving no education (RR 0.36, 95% CI 0.23 to 0.56). Regarding the health-related quality of life, the heterogeneity of measures applied in the studies included in this meta-analysis made it impossible to find consistent evidence. However, there is limited information regarding the improvement of some domain scores. There was no difference in the outcomes for total mortality, fatal and/or non-fatal MI, total revascularizations, and hospitalizations.
This paper has some limitations. First, the group of patients analyzed had a defective distribution between the two genders (male/female sex ratio = 2.62), which limits the generalization to the general population. This is due to the fact that sex is a risk factor for CAD, including ACS [30] which led to a preponderance of male patients in our study [31]. Secondly, we searched in the databases only for articles published in English. Thirdly, the comparison with placebo does not apply to psychological and educational interventions, and in all trials the control group was the usual care one. Thus, the nonspecific effects of psychotherapy and education were not accounted for. Fourth, we did not investigate intervention for other emotional disorders such as bipolar disorder. As in any systematic review, there may be a publication bias and the overall picture may be based on positive results, it being 8known that unsuccessful studies do not end up being published. Finally, there are some important gaps in the literature. It is important to emphasize that the findings are limited by the paucity of randomized controlled trials that have studied psychoeducational intervention exclusively in patients with ACS. Psychoeducational interventions were varied in terms of the type of intervention, the number of sessions and the total duration, the enrolled population, and the setting (phone or in person or both). Therefore, there is no possibility of a meta-analysis, mainly due to the heterogeneity of outcomes and their measurement tools.
Psychoeducational rehabilitation appears valuable in ACS, being associated with improvement in new non-cardiovascular events, quality of life, most cardiovascular risk factors, physical behavior, and mental health outcomes such as depression, anxiety, and distress, along with illness perception and cognitions. In contrast, most interventions proved a lack of enhancing diastolic blood pressure, blood glucose level, body mass index, abdominal circumference, and self-esteem. MACEs and rehospitalizations at 1 year after psychotherapies were significantly reduced, but this improvement was not maintained at 5-year follow-up.
In the era of personalized medicine, patients with ACS should benefit from specific psychoeducational strategies and the choice of the type of intervention should be chosen in accordance with the evidence-based guidelines. Unfortunately, there are currently a limited number of clinical trials that have studied the effect of psychoeducation focused on MI. Taking into account the heterogeneity issue of these studies available in the literature at the moment, we highlight the need for large RCTs with structured integrated multi-modality psychological interventions with a detailed methodology of implementation. Moreover, there is a critical need to establish a number of sessions and a total dose standardized by experts in the field, but this requires further studies. Given the possible health consequences and significant costs of untreated emotional disorders (especially depression) in patients with heart disease, there is a necessity for RCTs to evaluate the impact of psychotherapy on cardiac morbidity and mortality.